With the widespread outrage over the astronomical price increase of Epi-Pens, essential for those with severe allergies, attention has turned to other critical prescription drugs, especially insulin. Insulin is a necessity for those with Type 1 diabetes, a condition where the pancreas no longer produces insulin. The rising cost of insulin makes it increasingly difficult for those without insurance or substantial incomes to afford this life-saving medication, putting their lives or their children’s lives at risk.
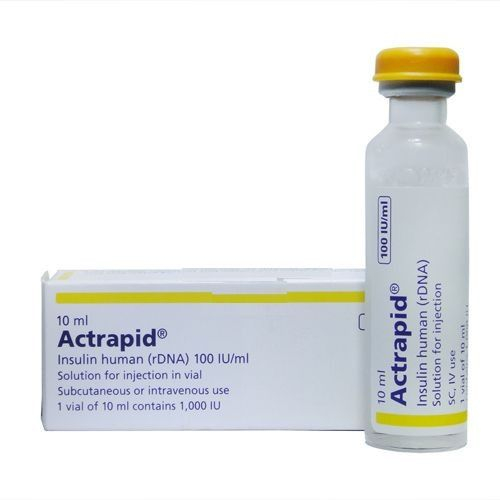
My nephew, who has Type 1 diabetes, requires four vials of short-acting insulin (bolus) monthly. Without insurance, these would cost nearly $1,200. My niece, also a Type 1 diabetic, needs one vial of long-acting (basal) insulin a month, which would cost well over $350 without insurance. This reality starkly contrasts with the intentions of the scientists who discovered insulin 95 years ago, who envisioned it being available to everyone in need.
History of Insulin
In 1921, Dr. Frederick Banting and Charles Best made the most significant discovery of their careers: insulin. At the time, they could not foresee how vital this discovery would become or the countless lives it would save. Before the discovery of insulin, diabetes was a death sentence. Adults and children diagnosed with the disease were lucky to live a few short months before succumbing to it. The only available treatment was a starvation diet, which offered little relief and prolonged suffering. In 1921, Banting and Best’s discovery changed the lives of those diagnosed with diabetes forever.
Dr. Banting and Charles Best were clear that their creation of insulin was meant to help those in need, not to generate profit. They sold the patent to the University of Toronto for only $1, hoping that this would ensure insulin would be accessible and affordable for all diabetics.
Fast Forward to Today
Nearly 96 years after the groundbreaking discovery of insulin and the altruistic gesture by Banting and Best, who sold the patent for just $1, the insulin industry has evolved into a colossal $25-billion-dollar market globally. This figure is projected to nearly double, reaching over $48 billion by 2020. The continuous price hikes of insulin have sparked a complex debate about the various factors contributing to this situation.
While it might be easy to cast blame solely on pharmaceutical companies for the exorbitant costs of insulin, the reality is more intricate. Pharmaceutical companies are indeed a significant part of the equation, but they represent only one piece of a larger puzzle. The true cost of manufacturing insulin remains one of the industry’s most closely guarded secrets, and the role of health insurance companies also adds layers of complexity to the pricing structure.
Playing devil’s advocate, it is important to recognize that pharmaceutical companies turning a profit is not inherently negative. A portion of their earnings is reinvested into research and development, leading to advancements in insulin formulations. These improvements aim to create more effective and efficient insulin products, ultimately benefiting patients in the long run. However, this raises a critical question: to what extent is it justifiable for these companies to make substantial profits when so many individuals struggle to afford the medication they need to survive?
The increasing commercialization of insulin highlights a significant ethical dilemma. On one hand, innovation and progress in medical research are driven by the profits pharmaceutical companies generate. These funds enable ongoing improvements in diabetes treatment, potentially leading to better health outcomes for patients. On the other hand, the steep prices place a severe financial burden on those who depend on insulin for their very survival.
Moreover, the involvement of health insurance companies in the pricing structure of insulin adds another layer of complexity. Insurance plans often determine the out-of-pocket costs for patients, and the variability in coverage can lead to significant disparities in what individuals pay for their medication. Those without insurance or with inadequate coverage are left to bear the full brunt of these high costs, exacerbating the financial strain and potentially leading to life-threatening situations where insulin is rationed or skipped altogether.
The disparity in insulin accessibility raises urgent questions about the balance between profit and public health. While the reinvestment of profits into research is a necessary component for medical advancement, it should not come at the cost of making life-saving medications inaccessible to those in need. There must be a middle ground where pharmaceutical companies can continue to innovate without pricing their products beyond the reach of ordinary people. This complex situation calls for a multi-faceted approach to address the high costs of insulin. Transparency in manufacturing costs, regulation of pharmaceutical pricing, and more equitable insurance coverage are all critical elements that need to be considered. Only through a collaborative effort involving policymakers, pharmaceutical companies, and the healthcare industry can a sustainable solution be found.
Prescription Medicine Prices
The pricing of insulin begins at the pharmaceutical companies, where they set the price based on various formulas, algorithms, and strategic decisions. These decisions are influenced by multiple factors, including the anticipated sales volume and the competitive landscape of the diabetes industry. Being a for-profit sector, the costs of medications and essential supplies for managing diabetes are subject to increase, especially if sales do not meet company expectations. Additionally, when new companies enter the market, competition can drive prices higher rather than lower, as might be expected. The myriad factors contributing to these price increases can be overwhelming, leaving consumers struggling to understand why their necessary medications are becoming more expensive.
The diabetes industry’s competitive nature and profit-driven model significantly impact the cost of insulin and other diabetes management supplies. When a company anticipates lower sales, it might raise prices to meet its revenue targets. Conversely, increased competition could lead to price hikes as companies strive to maintain or increase their market share. These dynamics result in a complex and often opaque pricing structure that ultimately burdens the patients who rely on these medications.
Moreover, the lack of transparency in manufacturing costs adds another layer of complexity. Patients and advocacy groups frequently call for more openness about how prices are set and the actual costs involved in producing insulin. Without this transparency, it is challenging to hold pharmaceutical companies accountable or push for fair pricing that considers the financial realities of those living with diabetes.
Risky Behaviors to Stay Alive
The escalating prices of insulin have forced many people with Type 1 and Type 2 diabetes into dangerous behaviors as they struggle to afford their medication. One common coping strategy is rationing insulin doses, taking less than prescribed to stretch their supply. This practice can lead to severe health complications, including hyperglycemia (high blood sugar) and, in extreme cases, diabetic ketoacidosis (DKA), a potentially fatal condition.
Some patients face heart-wrenching choices, such as skipping doses or not filling their prescriptions due to financial constraints. Others may sacrifice essential needs, like food and other groceries, to afford their insulin. These desperate measures are not just detrimental to their health but also raise profound ethical questions about access to essential medications. The high cost of insulin puts patients in a perilous position, where staying alive becomes a game of chance. The decision to ration medication or forgo necessities to afford insulin underscores a glaring issue in the healthcare system. The fundamental question arises: When did it become acceptable to place such a heavy financial burden on individuals for a life-sustaining medication?
Pharmaceutical companies, like any business, aim to make a profit. However, the ethical implications of exorbitant pricing for essential medicines cannot be ignored. Insulin is not a luxury; it is a necessity for survival. The practice of overcharging for such a critical medication raises serious concerns about the balance between profit and public health.
The financial strain caused by high insulin prices has far-reaching consequences. Patients who cannot afford their medication are more likely to experience severe health complications, which can lead to increased hospitalizations and long-term health issues. This not only affects their quality of life but also imposes additional costs on the healthcare system.
When did it become acceptable and ethical for companies to assign a price not only to my sister’s children’s lives but also to the quality of their lives?
That is the question I genuinely seek an answer to.
References:
- National Institute of Diabetes and Digestive and Kidney Diseases
- Centers for Disease Control and Prevention: Diabetes Risk Factors
- Centers for Disease Control and Prevention: Preventing Diabetes Complications